With so much recent publicity surrounding gene therapy, it’s no surprise that the topic was a major focus of the recent 2019 NORD Rare Diseases & Orphan Products Breakthrough Summit.
From diagnosis and clinical trial design to manufacturing, pricing strategies, and ethical concerns, gene therapy — both its high costs and limitless potential for curing diseases — generated much discussion at the Washington, D.C., event, which was organized by the National Organization for Rare Disorders (NORD) and attended by more than 900 delegates Oct. 21–22.
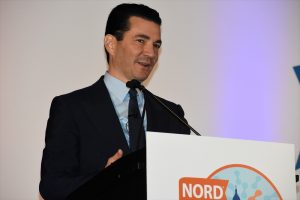
“On one hand, this is a splendid time to be doing what we do,” said Scott Gottlieb, MD, former commissioner of the U.S. Food and Drug Administration (FDA), and now a partner at Washington-based New Enterprise Associates. “On the other hand, it’s imperative that all patients have access [to these new therapies], regardless of someone’s ability to afford them. Many of the treatments are so dramatic, they can quite literally alter the destiny of someone’s life.
He regarded his leadership of the agency, from May 2017 to April 2019, as “a wonderful time at the FDA because we had the benefit of cures and new money as a tailwind, but also in large measure because of the opportunities before us — such as gene therapy and CRISPR — to fundamentally alter diseases.”
Gottlieb’s comments come toward the end of a year that saw the FDA approve the Novartis treatment Zolgensma, the first gene therapy for spinal muscular atrophy (SMA). With a price tag of $2.1 million, it’s the most expensive medication in history.
“When it comes to curative therapies, it’s not that we can’t sustain the cost of a million-dollar therapy if it means curing a pediatric disorder. We can afford that,” he said. “But what we can’t afford is to let an insurance company determine your child’s destiny.”
While there’s a “real sense of excitement” about gene therapy for illnesses such as hemophilia, SMA, sickle cell disease, and Duchenne muscular dystrophy, these expensive new treatments may actually accentuate rather than reduce disparities among patients, said Steven Pearson, MD, founder and president of the Boston-based Institute for Clinical and Economic Review.
“There’s a real anxiety that this wave of innovation will lead to unexpected high costs,” he said. “Insurance companies are writing policies today that will exclude gene therapies. That’s ridiculous. It doesn’t help anybody.”
Fair pricing strategies
Fair pricing strategies are badly needed to ensure that all who need future gene therapies will have access to them, regardless of the cost, said Pearson, whose independent, nonpartisan agency objectively evaluates the clinical and economic value of prescription medications.
“We could just give this to the federal government and create risk pools, but I think the private market can sort this out,” he said. “A fair price should never mean that a patient should have to repeat their genetic tests every six months to show they still have the same bloody condition.”

During a panel, titled “Gene Therapy: Overcoming Challenges for Both Patients and Manufacturers,” pharmaceutical executives and patient advocates discussed what the coming scientific revolution means for them.
Gene therapy offers the possibility for kids with devastating conditions and severely limited life spans to live long, productive lives and fulfill their potential, said Mark Rothera, president and CEO of London-based Orchard Therapeutics, who moderated the panel.
Rothera said he’s worked in rare diseases since the late 1980s, and has launched seven orphan drugs in his career.
“But I joined Orchard a few years ago because I’ve never seen data like this before. It’s taken 20 or 30 years of work to get to this point,” he said. “The whole system is geared up for chronic long-term therapy. Now we’re talking about one single intervention that will deliver lifelong benefits, so the system has to welcome that and adapt to it.”
The panel included Olivier Danos, PhD, senior vice president and chief scientific officer at Regenxbio; Neil Horikoshi, CEO and executive director of the Aplastic Anemia & MDS International Foundation; Stephanie Uder, vice-president of product management at Accredo; and Amy Price, outreach coordinator at the Leukodystrophy Family Forum.
“You can imagine the enormous financial and emotional toll that 24/7 care takes on moms and dads,” Rothera said. “Maybe one of the parents has to give up a job to be there. Imagine if that’s no longer required, because the parents have a healthy child, and can use that time and energy to look after healthy children.”
Gene therapy for ADA
To that end, Orchard is focused solely on treating children with primary immune deficiencies, neurometabolic disorders, and hemoglobinopathies — most of which lack treatments today.
The company’s pipeline includes Strimvelis, the first ex vivo autologous gene therapy to treat patients with severe combined immunodeficiency due to adenosine deaminase deficiency (ADA) for whom no suitable stem cell donor is available. Approved by the European Medicines Agency in 2016, Strimvelis was acquired by Orchard from GlaxoSmithKline in March 2018.

ADA affects about 15 people per year in Europe and 12 per year in the United States. Strimvelis retails for $780,000, compared to $4.25 million for 10 years of weekly enzyme replacement therapy.
“We’re building a company on a global scale to bring these medicines to patients around the world as quickly as we can, but we face plenty of challenges with patient identification,” Rothera said. “When you’re bringing gene therapy for the first time in the world to a community that hasn’t had treatment, there’s been less of an effort at diagnosis.”
“But time also matters,” he added. “Some patients, you want to treat as early as possible before symptoms develop — so newborn screening is very important.”
Rothera also noted the complicated logistics of bringing patients from all over the world to a specific hospital to receive gene therapy.
“Imagine the case of a child born with a rare disease that has been cured through one single intervention,” he said. “Effectively, that child is no longer a patient — yet will need a further 15 years of follow-up. A procedure like this requires exquisite coordination. The patient’s own cells become the product.”
Flying abroad for gene therapy
Amy Price knows about the complicated logistics of traveling across the ocean to cure a child.
She and her husband, Brad, have three children with metachromatic leukodystrophy (MLD). The disease affects white matter in the brain, causing progressive loss of mobility and sensation as well as intellectual decline.

Their daughter, Liviana, was born in January 2008 and diagnosed with MLD in December 2010. Giovanni was born in January 2010. After genetic testing revealed that he also had the disease, the boy was accepted into a clinical trial at Italy’s San Raffaele Telethon Institute for Gene Therapy in Milan. He was treated in 2011, though it was too late for Liviana, who died in 2013.
The following year, Price gave birth to triplets. One of them, Cecilia, inherited MLD and got the gene therapy in Italy at 9 months old. According to a post in the PLOS Blogs Network, the gene therapy that Giovanni and Cecilia received “adds corrected genes for the enzyme arylsulfatase A to bone marrow stem cells taken from the children. The cells are infused and migrate to the brain, where they give rise to corrected glial cells that make the necessary enzyme. Done early enough, symptoms never begin.”
A psychologist, Price recently interviewed 16 families whose children — 12 with MLD — underwent gene therapy treatments, mostly between 2011 and 2016. Half of the children was American and the other half was European. Their ages ranged from 8 months to 11 years, with an average age of 3 years.
She found that the most formidable challenges for families were fear of unknown or long-term treatment outcomes; family separation; having to care for other children at the same time; social isolation; unfamiliar language or customs; and financial well-being.
“It seems like such a small thing, but if you don’t have WiFi and nobody speaks your language, it’s a cumulative effect,” said Price, noting the emotional and physical stress of travel logistics, flying, and general exhaustion on the patients and their families.
Among her suggestions:
- Bring patient communities into the preclinical planning process.
- Understand and effectively address cultural challenges with international participants.
- Identify and work to eliminate the external stressors that impact families (lack of WiFi, social and language barriers).
- Provide effective psychological support during and after hospitalization, and connect patient to local resources.
- Provide clinical follow-up at local hospitals to eliminate the challenges of traveling.
“There is so much unknown with a new treatment, and the patients make an immeasurable and priceless sacrifice of hope,” said Price. But even so, she added, “it’s a life-or-death choice, and 100% [of respondents] said they would do it again.”

